For weeks ahead of the 2021 AICR Research Conference, I was eagerly looking forward to the session, “What can we tell our patients?”. As a registered dietitian nutritionist, I love learning about advances in research on the influence of diet, physical activity and weight on cancer risk and cancer survivorship. Yet it’s the practical implications for how lives can be improved that especially excite me.
When it comes to lifestyle choices and cancer, consider the “known knowns,” the “known unknowns,” and the “unknown unknowns.”
That was the advice of Wendy Demark-Wahnefried, PhD, RD, as she began her presentation.
Health professionals want to share recommendations supported by the strongest available research. That’s what Demark-Wahnefried meant by the “known knowns.”
But awareness of all three should shape what health professionals communicate and how we address questions about cancer risk and survivorship. For example, conference sessions on the “microenvironment” within the body immediately surrounding a cancer, the gut microbiome’s potential far-reaching effects and studies about weight loss after cancer explored questions we can’t yet fully answer. These are examples of “known unknowns” that exist, even as progress in research means that we are learning more than ever before.
And the “unknown unknowns”? Simply remembering that we do not yet have all the answers becomes a crucial element in responding to patients’ questions about claims they encounter in media and advertisements. For example, there could be unexpected effects of supplements or diets bearing “anti-cancer” claims based only on laboratory studies.
Let’s explore what this approach looks like while reviewing research updates presented at the AICR conference.
Start Here: What We Need to Communicate About Cancer
Evidence supporting the AICR Cancer Prevention Recommendations continues to be strong. Even as emerging evidence explores nuances in how individual variations in the Recommendations may call for modest differences in their application, these Recommendations remain the crucial message. Media headlines can be like a bright shiny ball, distracting people’s attention to novel studies. But the Recommendations were built on evidence strong enough that the advice was deemed unlikely to change. And indeed, even with new insights presented at the conference, evidence continues to support the AICR Cancer Prevention Recommendations as the blueprint for a health-protective lifestyle.
Maintain a Healthy Weight and Avoid Weight Gain in Adult Life
Like pieces of a jigsaw puzzle, evidence from laboratory studies, long-term population studies and controlled human trials fits together to provide more support than ever about excess body fat and adult weight gain as one of the most powerful influences on cancer risk and outcome.
- Breast tissue’s microenvironment can undergo obesity-related changes that play major roles in the strong association of post-menopausal breast cancer and obesity. With weight gain, expanded fat cells in the breast can lead to local inflammation and elevated levels of estrogen, insulin and growth factors. Research is in progress exploring the implications for breast cancer treatment and for women at increased risk due to inherited mutations in BRCA1 or BRCA2 genes.
- Hepatocellular carcinoma (HCC, by far the most common form of liver cancer) is on the rise. People may be aware of HCC caused by viral infection (HBV or HCV) or by alcohol-related cirrhosis. But Rohit Loomba, MD, MHSc, presented research showing that in the U.S., 20–25% of HCC is now attributed to non-alcoholic fatty liver disease (NAFLD), a condition associated with excess body fat. Loomba shared research showing that modest weight loss before cancer develops can improve liver damage.
- Body mass index (BMI) remains the metric best suited to represent weight and adiposity in large population studies. But research is progressing in identifying factors like inflammation, insulin and growth factor signaling pathways as the mechanisms through which dysfunctional body fat exerts its harms. So, on an individual basis, we need to consider that relying only on BMI to define “healthy” could miss people at risk.
Diet Quality and Plant-Forward Eating Both Matter
Advances in research continue pointing to a pattern of plant-focused eating as a key strategy for lower cancer risk and better overall outcomes after a cancer diagnosis.
- A plant-based diet does not automatically qualify as a high-quality diet. If eating habits focus around highly processed plant foods that are low in fiber and high in added sugars or refined grains, they aren’t providing the array of vitamins, minerals and phytochemicals that combine to protect body cells.
- Diet quality is associated with lower risk of cancer incidence and cancer mortality—and fewer deaths from cancer and all causes combined in cancer survivors. That means choosing vegetables, fruits, whole grains and beans (including dried beans, lentils and soy foods) for the largest portion of your plate at each meal. Whether or not you want to also include dairy products, fish, poultry and unprocessed red meat, these fiber-rich foods deserve center stage, with low amounts of added sugars, unhealthy fats and sodium.
- People living with and beyond cancer often already have or develop conditions like cardiovascular disease or type 2 diabetes. That makes the combination of diet quality AND plant-focus important to support better overall health.
Physical Activity Is Vital Regardless of Weight
Physical activity is misunderstood. For many people, it’s either for weight loss or for sports. And if you don’t consider yourself an athlete or don’t lose weight after a week of exercise (as most people would not), it’s easy to write it off. Health professionals have a vital role in changing that.
- Regular physical activity is associated with lower risk of developing cancer (especially breast, colorectal and endometrial cancers) and likely with lower mortality rates among people who get cancer. That’s even after statistically adjusting for age, weight and other influences. Since findings are from observational studies, research in controlled trials is ongoing regarding cancer outcomes.
- Physical activity may regulate the microenvironment immediately surrounding cancer cells in addition to its well-established effects on factors like insulin resistance throughout the body. In animal models, moderate amounts of physical activity cause about a 30% decrease in tumor growth. Lee Jones, PhD, shared research on the effects of exercise both within cancer cells and in the tumor microenvironment.
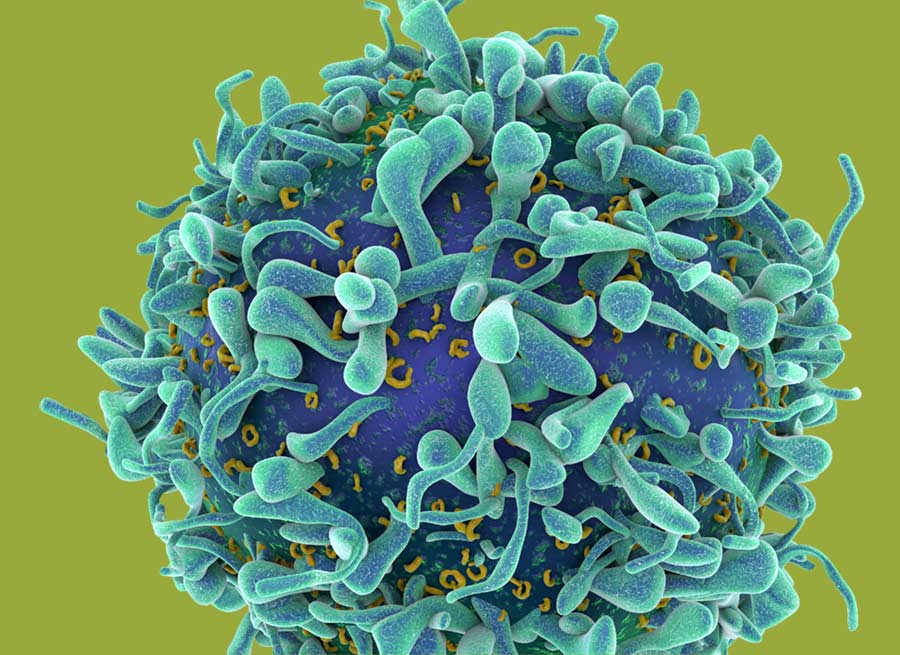
- Each bout of exercise matters, causing an almost instant release of immune cells. For example, natural killer cells, which show some of the largest increases, are powerful anti-tumor cells. Laboratory studies reviewed by Richard Simpson, PhD, show that these increased immune cells track toward cancerous tumors and inhibit their growth. Research is underway exploring how exercise might be added to support immunotherapy cancer treatments.
Health-Care Professionals: 3 Ways to Help Your Patients Now
People listen to their health-care professionals. Amid mountains of information people encounter, health-care professionals play a critical role in helping people identify what is worth their attention and how to put it in practice.
- Talk about strength of evidence is key to deciding about where to focus. For medical treatments, randomized controlled trials are the gold standard. But Edward Giovannucci, MD, ScD, explained that for a disease like cancer that develops over many years, they are prone to miss true associations with diet.
- Discuss cancer screening with an individualized perspective. Surveys show that many people with overweight or obesity, metabolic syndrome or other cancer risk factors do not recognize their risk. Explain in non-judgmental terms that although these conditions have become common, that does not mean they are healthy. For example, amid the increase in early-onset colorectal cancer, the recommended age to begin screening is now lower.
- Ask cancer survivors about barriers to a healthy lifestyle. After a cancer diagnosis, lack of exercise and unhealthy eating choices are common. Discuss the physical, psychological and social obstacles encountered, and what resources are available to help people overcome them.
What’s Ahead Amid the Many “Unknowns”?
Medical therapy for cancer has progressed from the few general treatment options of yesteryear to precision treatments optimized for individual cancer types. Neil Iyengar, MD, predicted in his presentation that we are moving toward “precision nutrition,” in which choices for diet, physical activity and weight maintenance or change may someday be geared to match different cancer or treatment types. For now, however, this remains in the realm of “known unknowns.” Before we promote tentative findings prematurely, we must remember that there are still many “unknown unknowns”—consequences of those strategies of which we are currently unaware.
Dr. Iyengar, echoed by many other researchers during their presentations, emphasized that for now, the steps highlighted by the AICR Cancer Prevention Recommendations remain today’s best advice. As health professionals, these remain our key messages and the goals to which we need to help our patients progress.