The Road Ahead
If you are diagnosed with cancer, knowing what to expect during treatment may help cut through the confusion and stress. It can be helpful to speak in detail with your doctor, ask questions, and thoroughly evaluate your treatment options. Information can help you understand what’s in front of you, and can empower you to better advocate for your own health.
Introduction to Treatment Options
There are a number of options for cancer treatment. Although courses of action will vary depending on the diagnosis, generally speaking, most options for cancer treatment include surgery, radiation therapy, chemotherapy, and targeted or biological therapies. Some healthcare professionals will also recommend a blend of complementary/alternative therapies (“integrative therapies”), such as meditation, visualization, massage, and acupuncture.
There is no one “best” method for treating cancers. Physicians usually deploy a combination of treatments, and tailor their approach to account for the type, stage and location of the cancer, and to suit the health of the specific patient. Regardless of the type of treatment, the goal is the same: to stop the uncontrolled growth of cancer cells with as few harmful side effects as possible.
Below is a brief description of the various treatment methods.
Surgery removes the tumor and any nearby tissue that may contain cancer cells. Sometimes, healthy tissue around the tumor has to be removed to help keep the cancer from spreading. Possible short and long-term side effects depend on the location and extent of surgery.
In radiation therapy (also called x-ray therapy, radiotherapy, brachytherapy or irradiation), high-energy rays are used to damage cancer cells so they are unable to grow and multiply. Radiation therapy is directed only to a specific area of the body where treatment is needed. As a result, it generally causes side effects that are limited to one area, most of which are not permanent. The common side effects are fatigue and skin rashes or redness in the area being treated. In some cases, radiation therapy may cause a decrease in the type of blood cells that help protect the body against infection, bleeding and anemia.
Chemotherapy is the most common treatment for cancer. There are many types of chemotherapy drugs, and the type and stage of cancer determines which ones are used. Often, more than one drug is used during a single course of treatment, and many chemotherapy drugs are applied in combination with surgery, radiation and hormonal therapies. Chemotherapy drugs target cancer cells, but can have toxic effects on healthy cells, and temporary side effects can occur. Unlike radiation therapy, chemotherapy may affect cells in several parts of your body as the drugs travel through the bloodstream. Common side effects include fatigue, hair loss, nausea and vomiting, and loss of appetite. Other side effects include an increased chance of infection, bleeding and anemia due to a decrease in normal blood cells. It may take several months to recover from many of the side effects of chemotherapy, and even longer for some symptoms. Talk to your doctor about ways of coping and if referral to another health care practitioner (such as a dietitian or physical therapist) can help.
Some types of cancer are affected by hormones that fuel the growth of cancer cells. For these cancers, your doctor may recommend medications that block cancer cells from getting the hormones that feed cell growth. Hormone therapy can cause a number of side effects, depending on the intervention. In some cases, a treatment interferes with the body’s normal production or use of hormones. For example, women taking tamoxifen may experience some symptoms of menopause, such as hot flashes. Although rare, some patients may have nausea and vomiting, swelling, increased appetite and weight gain. Because some hormone medications cause an increase in appetite, they are occasionally prescribed for patients with weight loss or a reduced appetite.
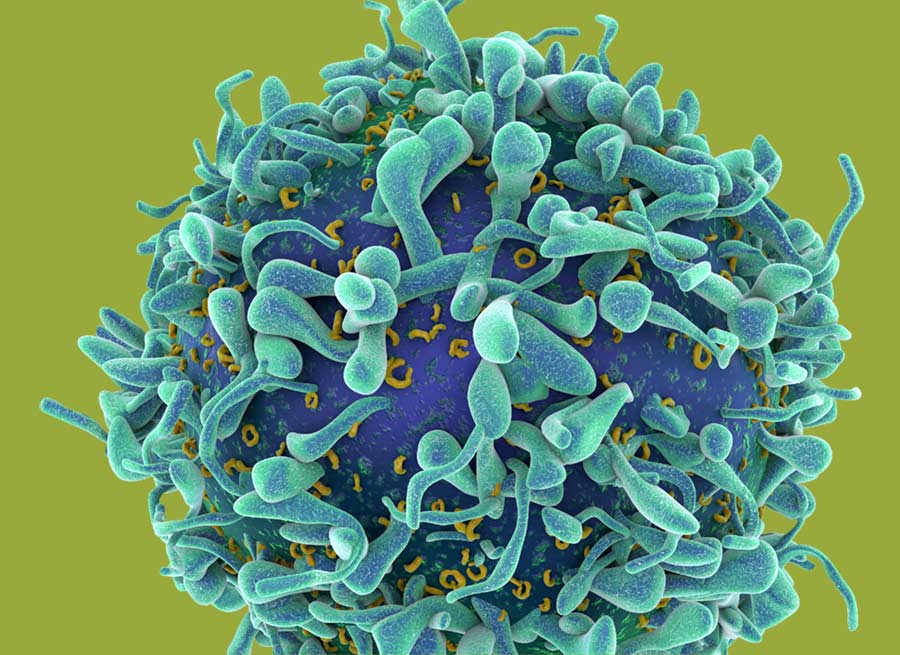
Targeted therapy involves the use of drugs that are targeted against specific messages sent by cancer cells to help them grow. Targeted therapies include biologic, immunologic and gene therapy. Many of these treatments are considered investigational because they are still under study, and their effectiveness has not been proven.
To determine the safety and effectiveness of a targeted therapy, it is studied in a clinical trial—a carefully controlled study that often compares the new therapy with standard treatment methods. Sometimes the investigational treatment is not helpful, but other times it can lead to significant improvements in health and quality of life. Patients who participate in clinical trials make an important contribution to the advancement of medical science and cancer care.
- Biologic Therapy
Biologic agents target specific message systems within cancer cells that send signals to turn on cell growth. Some biologic agents have been approved for treating cancer in combination with chemotherapy agents. Many others are being studied to block different growth pathways of cancer cells. Side effects depend on the type of treatment. Some treatments can damage the heart muscle. Others can cause flu-like symptoms, such as fever, chills, nausea, vomiting, fatigue and skin rashes. - Immunotherapy
Immunotherapy focuses on using the body’s immune system to help fight cancer or lessen treatment side effects. - Gene Therapy
Initiated in the 1990s, gene therapy replaces an active cancer-causing gene, also known as an oncogene, with a normal gene. Gene therapy might also involve removing bone marrow from a cancer patient, inserting a “designer” gene, and then returning bone marrow to the patient. At present, there are a number of serious obstacles that need to be overcome before this process is routinely available.
Also referred to as “complementary therapies,” integrative therapies do not replace conventional therapies, but may be used to provide added benefits. Popular complementary therapies include acupuncture,mind-body therapies, botanicals/herbals, antioxidants/dietary supplements, and special diets.
While certain complementary therapies for cancer may appear to help some people, scientific evidence proving their effectiveness is often lacking. And some of these therapies may be harmful and may dangerously interact and interfere with conventional treatments. Be informed about the therapies you are considering using, and always approach unconventional, complementary and alternative cancer therapies with caution. Keep in mind that just because a therapy is “natural,” it is not guaranteed to be harmless. These therapies should complement, but never replace, traditional medical approaches to cancer treatment. To protect your well-being, always inform your physician about any complementary therapies, such as supplements, you are using.
Questions About Your Diagnosis
As we live longer, more and more people are likely to get cancer. There are, however, millions of Americans who have been diagnosed and successfully treated for cancer. Improved screening and treatment methods have led to many people becoming long-term survivors.
Being an informed, involved patient is an important part in overcoming cancer. If you—or a loved one—has been diagnosed with cancer, here are answers to questions you may have.
Although the term “cancer” is often used as if it were one disease, cancer is actually a group of more than 100 different diseases affecting various parts of the body. They all have one common characteristic – the uncontrolled growth and spread of abnormal cells. These cells can multiply, form a tumor, and invade and damage healthy body tissues and organs.
Cancer is rarely caused by a single factor; rather, it is the result of a complex interaction between cancer-causing substances called carcinogens, DNA mutations and heredity. The process begins with the many thousands of genes found in each cell of the human body. Genes, made up of DNA, carry instructions for making the proteins that regulate all body processes, including how efficiently we process foods, metabolize toxins and fight infections.
Genes are activated, or switched on and off, by signals in the body or by environmental influences. For instance, alcohol, cigarette smoke, too much sun, or high levels of certain chemicals can damage DNA and cause genes to mutate, or change. When the body’s normal repair mechanism doesn’t work properly, because of genetic or environmentally caused mutation, the damaged cell continues to grow and multiply abnormally and can eventually lead to cancer.
Many people believe that all cancers are triggered by defective genes. However, most people who get cancer do not inherit altered, or mutated, genes. Only about 5 to 10 percent of all cancers are thought to be caused by an inherited “cancer gene.” Even if there is a strong family history of a particular cancer, it does not mean that cancer is inevitable. Dietary and lifestyle factors can interact with genes to influence whether an individual develops the disease.
One important consideration in cancer treatment is deciding on a doctor. You can find a board-certified oncologist by researching online and by asking your primary care physician, managed-care representative or a hospital’s oncology department. You must feel confident that your oncologist is not only experienced, but also competent and up-to-date, and that he or she sees you as a partner in your treatment.
Download AICR’s CancerResource (below) for a list of questions to ask your doctor that you can print and take with you.
When visiting an oncologist, it may lessen your anxiety to bring a list of questions and to take notes. It’s a good idea to bring a family member or close friend who may catch something you might miss – and ask questions too. Be sure you feel comfortable having an open discussion with your provider. Good communication is critical to a doctor-patient relationship and empowers you to have an active role in your treatment.
Even if you are satisfied with your health team, a second opinion can be useful. It can give you confidence in the information you have already obtained or it may offer a different approach to treatment.
It’s important to understand the diagnosis you receive when you visit your doctor. Powerful emotions – including denial, anger, fear, stress, loneliness, depression and hope – are natural responses to even a potential diagnosis of cancer. Getting the facts about your situation will help you make informed decisions in the days ahead. If you are nervous or don’t think you’ll remember what you are being told, bring someone with you, ask your doctor to write out the information you need, or take notes. Don’t be afraid to ask questions. Make sure you understand what the doctor is saying.
As you cope with the issues associated with a cancer diagnosis, including the effects on your roles and family routines, speak openly about your feelings. If you or family members are having trouble adjusting to the diagnosis, consider seeking referrals to local support organizations for help. Many people find that cancer support groups or conversations with another survivor with a similar diagnosis and treatment are sources of strength and can offer practical suggestions for everyday life.
Questions to Ask Your Doctor About Your Treatment
When you have been diagnosed with cancer, it’s important you understand your treatment options and care. Here are some questions you may want to ask your doctor or other member of your health care team.
What is your experience with treating this type of cancer?
What kinds of treatment do you recommend and why?
Are clinical trials or investigational agents an option for me?
What are the chances that the treatment(s) you suggest will be successful?
How long is treatment-typically?
What are the side effects of the treatment?
How do you determine if symptoms I am experiencing are normal or adverse responses to the medications or treatment?
What will my quality of life be during and after treatment?
Who is available for medical questions when you are not?
Is a nurse or other health care professional available to deal with phone inquiries?
What is the schedule for follow-up and post-treatment?
When do you generally return phone calls?
What is the cost of treatment, and is it covered by my health plan?
Cancer Resource:
Living with Cancer
AICR knows how challenging a cancer diagnosis can be, and we know how overwhelming the search for reliable information can seem. Our detailed CancerResource Living with Cancer handbook offers patients and families a comprehensive resource hub for cancer care decisions. This easy-to-understand, evidence-based publication walks you through the steps you may take as you face cancer, and provides specific recommendations about eating and physical activity that can help you before, during and after treatment.

A Helping Hand
Other Programs and Resources
AICR offers you information and resources that can be used through every step of your cancer journey. Our programs, recipes and outreach can help you manage your health from treatment to recovery, and empower you to move confidently into the next chapter of your life.
The Next Chapter
As you navigate life post treatment, you may find yourself dealing with a new normal. You may find you have a new outlook and life, but also a new fear of a second diagnosis. Research suggests that the same evidence-based guidelines that help prevent cancer also help guard against its return. These lifestyle adjustments can help protect against additional serious illnesses like heart disease, stroke and diabetes.
Dealing With Weight Gain or Loss
Treatment side effects, changes in diet, and lack of activity are some of the reasons why many cancer patients experience unplanned weight loss or gain during treatment. Talking with your oncologist, dietitian or other health professional can help you identify individualized strategies.
Any attempt to lose weight should be done carefully to ensure that you are getting the food and nutrients you need.
You can work with your healthcare team and, ideally, a dietitian to lose weight. They can guide your efforts so you maintain your muscle, while losing body fat.
Choose mostly plant-based foods, including vegetables, fruits, whole grains and beans. These foods are high in nutrients and help you feel full but are low in calories and fat.
Choose no-calorie beverages such as water for most of your drinks, unless your doctor or dietitian has advised otherwise.
Make sure your portion sizes are appropriate for you. If your activity level has dropped, try eating smaller portions to see if your hunger is satisfied with less.
Address fatigue, depression, stress and boredom in ways that don’t involve eating. Sleep or rest rather than eat when tired.
Even a little physical activity can make a big difference so follow your physician’s advice about when and how you can be active.
Many friends and family members will offer help. In addition to allowing them to provide meals, offer suggestions like accompanying you on a walk or to an appointment, bringing books, or assisting with housework.
Do not rely on dietary supplements for weight loss due to the potential interaction with treatment and medications. Speak with your doctor about any supplements you are taking or considering taking.
The goal is to increase your calorie consumption with nutrient-packed foods to gain weight back gradually. Eat several mini-meals throughout the day if you find you can’t eat much at one time.
Foods that are concentrated in calories and nutrients include:
- Avocado
- Dried fruits (raisins, dried apricots, dried cranberries)
- Nuts, seeds and nut butters
- Bean dips or spreads
- Fruit dipped in peanut butter
- Whole-grain crackers with cheese
- High-calorie cereals (such as oatmeal, granola or whole grain options)
- Healthy oils (such as olive or canola) to stir-fry or sauté foods
- 100% fruit juices
- Nutritional supplement drinks
You can also drink your beverages between meals instead of during meals. This may leave more room for higher calorie food at meals.
If you’re feeling up to it, add strength training to your routine. This exercise will help ensure that you gain back muscle mass.
Preventing Recurrence, Secondary Cancers
There are now more people surviving and living well after cancer treatment than ever before. Yet in general, cancer survivors face the possibility of cancer recurrence and have a slightly increased risk of developing another cancer compared to those who have never been diagnosed.
If a cancer returns to the same area years after treatment, it is called a recurrence. If a cancer develops in another part of the body, it is a secondary cancer.
The risk of a recurrence or a secondary cancer depends upon many factors, including the type of cancer and age at diagnosis. The risk of another cancer developing is relatively small. Research shows that overall one to three percent of cancer survivors will develop a secondary cancer.
As a cancer survivor, the fear of recurrence and development of another cancer can be stressful. Talking with your healthcare team may help you manage this fear.
What causes some individuals diagnosed with a cancer to develop another cancer is unclear. That’s one reason it’s important to take action to reduce your risk. Taking steps like choosing a plant-based eating pattern, engaging in physical activity, and following up with your healthcare team about your survivorship plan can help.
Of course, following all the healthy living guidelines is no guarantee you will live cancer-free. Just like not following every recommendation to lower your cancer risk does not mean you are to blame if a cancer develops.
Choose to do what you can, when you can.
After treatment, AICR recommends that cancer survivors follow our recommendations for cancer prevention when and if you are able to do so. These recommendations also reduce the risk of other chronic diseases like diabetes and heart disease.

Healthy Eating
Recipes for Survivors
A healthy diet is a vital part of a cancer patient’s journey before, during and after treatment. Eating healthy can help prevent common side effects of cancer treatment such as weight loss, taste changes and loss of appetite. It can also help those undergoing treatment feel better and maintain healthy survivorship.
Going Through the Journey
Cancer treatments can affect you both physically and emotionally, and it’s common to experience a lot of ups and downs. While some people find they can lead an almost normal life during treatment, others find day-to-day routines all but impossible. What you eat and how much you move can affect how you feel, and may make treatment more bearable.
Exercising During Treatment
The old recommendation to “just get plenty of rest” during cancer treatment has been updated. Today, research suggests that exercise, when carefully monitored, can improve sleep, reduce fatigue and improve the quality of life of cancer patients. It’s important to speak to an exercise specialist or a member of your healthcare team who can help you adapt an appropriate exercise program for you.
The American College of Sports Medicine recommends that cancer survivors should avoid inactivity, even when undergoing treatment. They point out that individuals “should be as physically active as their abilities and conditions allow.”
When you are able aim for 150 minutes (2 1/2 hours) of moderate-intensity aerobic physical activity at least two days a week. Also include muscle-strengthening activities such as lifting weights or doing push ups 2 days a week. You may enjoy brisk walks outside while pumping hand weights.
Especially if you were not exercising regularly before your diagnosis, begin slowly and carefully. Build up your activity level step-by-step and keep your oncologist and other health providers informed. Of course, how much activity you’re able to do during treatment depends on many factors related to your specific diagnosis, treatment, age and fitness level. Ask your health care team for guidance.
Research is ongoing as to how much of a role physical activity plays in reducing recurrence and lengthening life. Among cancer patients, research suggests that moderate, supervised physical activity
may increase…
Quality of life
- Ability to do daily activities
- How far you can walk
- Immune system function
Muscle mass
Muscle strength and power
Aerobic fitness
Flexibility
And may decrease…
Fatigue
Nausea
Symptoms/side effects
Depression
Anxiety
Heart rate
- Resting blood pressure
Length of hospitalization
- Weight gain
Dealing With Treatment Side Effects
Fatigue is the most common side effect of cancer treatment. For some, fatigue may continue after treatment ends. It can significantly affect your quality of life and make it difficult to prepare and eat nourishing meals.
Temporarily rely on convenience products, like ready-to-eat foods, frozen dinners, frozen or canned fruits and vegetables, prepared pasta sauces and instant rice. Check labels for healthy choices – foods low in sodium and high in protein and fiber.
Keep healthy snacks on hand. Examples are dried fruits, cheese on whole-grain crackers and graham crackers.
Prepare food when you’re feeling best. Prepare large quantities of your favorite meals and freeze leftovers in meal-size portions. Make blended fruit and yogurt shakes that can be kept in the refrigerator.
Get help with meals from friends and family members. Phone for restaurant, grocery store delivery or carry-out. Have meals delivered by a service such as Meals on Wheels or order pre-prepared meal kits.
Drink plenty of fluids as recommended by your healthcare team.
Try to be physically active. Consistent research shows that regular activity can relieve fatigue and also enhance mood and appetite.
There are many different causes of fatigue, including depression and difficulty sleeping. Talk to your doctor about your fatigue, and any other related symptoms, to determine if you’d benefit from other treatments.
Weight loss and undernutrition are common due to loss of appetite and other factors that affect eating. When severe, your quality of life and the function of important body organs such as the heart, liver and kidneys are compromised, as is your ability to heal from surgery, chemotherapy and radiation side effects. Try these tips to boost your nutrition:
Eat several small meals a day instead of three large meals.
Eat high-protein foods first in your meal while your appetite is strongest – foods such as beans, chicken, fish, meat, yogurt and eggs.
Eat your largest meal when you feel hungriest, whether that’s at breakfast, lunch or dinner.
Keep food interesting by changing recipes and seasonings or eating at nice restaurants.
Keep favorite foods and high-calorie foods and beverages around the house and other places you go.
If you cannot take in enough nutrition with food, ask your health practitioner about blenderized drinks like milkshakes and smoothies, liquid or powdered commercial nutritional supplements, or the possibility of tube feeding. If your gastrointestinal tract is not functioning well, then total parenteral nutrition (TPN) may be appropriate to consider with your doctor. TPN provides nutrients directly into a vein.
Weight gain is commonly seen during treatment for breast and some other cancers, in women undergoing hormonal therapies, and as a result of “induced/early menopause” from chemotherapy. Weight gain may result in part from a change in diet and exercise routines, such as eating more due to stress or to control nausea and being less active due to fatigue. If steroids are part of your cancer treatment, they can be a powerful appetite stimulant.
You may gain weight due to fluid retention; if so, see below. Tell your doctor about weight gain, especially if you gain weight rapidly over just a few days, so the cause can be identified.
Eat vegetables, fruits, whole grains and beans and other foods that are high in fiber to help you feel full.
Pay attention to portion sizes, checking food labels and the serving sizes listed.
Love what you eat. Include and savor foods that you enjoy most so you feel satisfied.
Eat when you’re hungry and stop when you are comfortably full. Consider psychological counseling or medications if you find yourself eating to address feelings of stress, fear or depression, and find alternatives to eating out of boredom.
Engage in regular physical activity, which can help manage your weight and relieve your fatigue.
When patients gain weight during treatment without eating extra calories, the weight increase may be due to edema, or swelling. Certain common drugs such as prednisone and gabapentin can cause the body to retain too much fluid. Tell your health practitioner about rapid weight gain so he or she can determine the cause.
Drink plenty of water unless you have been specifically advised by your doctor to limit fluids.
Eat less salt and foods with less sodium such as fresh or frozen fruits and vegetables and unsalted or reduced-sodium snacks and soups. Replace processed foods such as cold cuts, which can be high in sodium, with alternatives.
Stay as physically active as possible.
Elevate your legs when resting.
If needed, your physician can prescribe medications to minimize fluid retention.
Nausea is a common side effect of cancer treatment. It can sometimes be accompanied by vomiting. Anticipation of a treatment session can cause nausea in some cases.
Tips
Eat small amounts of food often and slowly, instead of large meals. If nausea in the morning is a problem, keep crackers and soda at your bedside to nibble on before getting up.
Eat foods at room temperature or cooler, as hot food can aggravate nausea because of strong odors.
Eat sitting up, and rest sitting up or reclined with your head raised for about an hour after eating.
Drink beverages between meals instead of with a meal. Drink beverages cool or chilled and sip through a straw.
Rinse out your mouth before and after eating, and suck on a hard candy such as peppermint or lemon if you have a bad taste in your mouth.
Avoid triggers where possible by recognizing times, foods, smells or events that trigger your nausea and try to change your schedule or diet to avoid them.
If the smell of food or cooking nauseates you, try to keep the room well-ventilated; prepare meals that don’t require cooking; ask others to cook your meals or have meals delivered from Meals on Wheels or other similar services.
For nausea from radiation therapy or chemotherapy, eat bland, soft foods on treatment days and avoid eating for an hour or two before treatment. If you find that the anticipation of treatment causes nausea, practice relaxation or meditation techniques or another activity to distract yourself.
Discuss the use of anti-nausea medications with your doctor.
Foods to try:
Toast and crackers, yogurt, sherbet, popsicles, pretzels, angel food cake, canned fruits (peaches, pears, fruit cocktail), skinned chicken (baked, boiled), oatmeal and broths
Foods to avoid:
Any food that’s fatty, greasy, fried, spicy, very sweet and has a strong odor
Vomiting can follow nausea and can be brought on by some cancer treatments. Other factors can make vomiting worse such as food odors, gas in the stomach, or motion. Vomiting may occur without associated nausea. Tell your doctor if you have persistent vomiting and cannot keep liquids down. It is important to prevent dehydration if you are vomiting.
Tips
Sit upright and bend forward after vomiting.
Don’t eat or drink until your vomiting has subsided.
Once vomiting is under control, try drinking small amounts of clear liquids.
Try eating small amounts of soft foods when you are able to keep down clear liquids. And gradually work your way back to your regular diet.
Drinks to try:
Cranberry juice, cool broth or flat soda (carbonated beverages can lead to vomiting in some people)
Foods to try:
Soft foods such as cream of wheat, pudding, frozen yogurt and gelatin
Diarrhea is another possible side effect of cancer treatments, including chemotherapy and other medications, radiation therapy to the abdomen, and surgery. Other potential causes include infection, food sensitivity and emotional upset. Call your health practitioner if you have severe or long-term diarrhea, which may cause dehydration, nutrient loss and other health problems. Medications may be helpful.
Tips
Drink plenty of liquids, aiming for at least eight 8-ounce glasses each day. Good choices of fluids include water, diluted juice, broth and decaffeinated coffee or tea. Liquids at room temperature may be easier to tolerate.
Eat small amounts of food throughout the day rather than three large meals.
Some doctors recommend temporarily following a “BRAT” plan – a low-fiber regimen featuring bananas, rice, applesauce and toast – but its effectiveness is currently being reexamined. Check with your doctor.
Foods to try:
Rice, noodles, well cooked eggs, bananas, puréed vegetables, applesauce, white bread, skinned turkey or chicken, fish, mashed potatoes, yogurt, and kefir
Foods to avoid:
Raw vegetables and fruits; high-fiber vegetables, like broccoli, corn, beans, cabbage, cauliflower and peas; onions and strong spices; greasy, fatty and fried foods; alcoholic beverages, caffeine-containing beverages
Constipation can result from some cancer treatments and pain medications. Constipation can also happen if you are not eating enough fiber or drinking enough fluids. Relying on Tube feedings or physical inactivity for extended periods of time can also cause constipation.
Tips
Drink more liquids, aiming for at least eight 8-ounce glasses a day. Liquids can help keep stools soft. Good choices include water, prune juice, warm juices, decaffeinated teas and hot lemonade.
If you develop gas, limit certain foods. Culprit foods include broccoli, cabbage, cauliflower, beans, cucumbers, onions and carbonated drinks. Over-the-counter anti-gas products with simethicone may help you avoid discomfort from these foods. Always check with your doctor before self-medicating, even with over-the-counter medications.
Eat a large breakfast, including a hot drink and high-fiber foods (like hot or cold cereal, whole-wheat toast and fruit).
Increase your physical activity, aiming for a walk or other limited exercise every day.
Consider a fiber supplement or over-the-counter medications such as stool softeners or laxatives, if necessary. Always speak with your health practitioner first for specific guidance. Remember to drink plenty of fluids with such a supplement.
Drinks to try:
Water, prune juice, warm juices, decaffeinated teas and hot lemonade. Aim for at least eight 8-ounce glasses a day.
Foods to try:
High-fiber vegetables, like broccoli, corn, beans, cabbage, cauliflower and peas; whole-grain breads
Feeling full from a small amount of food can occur for a variety of reasons and is especially likely if you’ve had upper abdominal surgery. It is important to try to eat enough to allow you to strengthen your body and support healing. Your doctor may prescribe a medication to help.
Eat small meals throughout the day, keeping healthy between-meal snacks on hand.
Fortify your meals with calorie-rich, nutritious foods.
Avoid fried and greasy foods because fat lingers in your stomach longer than carbohydrates or protein. Avoid foods that give you gas.
Drink beverages between meals rather than during meals, so you feel less full while eating.
Rest after meals with your head elevated.
Ask a health professional about drinking blenderized drinks (milkshakes, smoothies) and liquid or powdered commercial meal replacement beverages to boost calories and nutrients.
Changes in how foods taste can result from chemotherapy, radiation therapy and the cancer itself. Some people experience bitter or metallic tastes, especially when eating high-protein foods such as meat. Each person’s sense of taste can be affected differently, and so the best approaches for minimizing the unpleasant taste and enhancing flavor can vary. It simply may take some time after treatment is completed for your sense of taste to return to normal.
Choose foods that appeal to you. Moist and naturally sweet foods such as frozen melon balls, grapes or orange wedges may be particularly appealing, as may tart foods and beverages such as oranges, lemon yogurt or lemonade (but not if your mouth is sore).
If the taste of red meat is now less appealing, find healthy alternatives, such as chicken, turkey, fish, beans, nut butters, eggs or dairy products.
Marinate meats in juice, teriyaki sauce, barbecue sauce, Italian dressing or other flavorful liquid you find appetizing.
Add small amounts of sugar to some foods, which may decrease salty, bitter or unpleasant tastes.
Serve foods cold or at room temperature, which may improve how they taste.
Brush your teeth and tongue and rinse your mouth regularly, especially before eating, to clean your taste buds. Choose alcohol-free mouthwashes; look at the label for inactive ingredients.
Rinse your mouth several times a day with water or a baking soda mixture (one quart water combined with one tablespoon baking soda).
Try sour candies.
People who digested milk and milk products easily before radiation or chemotherapy treatment may experience an intolerance resulting in cramps and diarrhea. This development is not common. For most people small amounts of dairy foods can still be tolerated.
Try small portions of milk, yogurt or cheese to see if you can tolerate them. Yogurts and aged cheeses may be easier to digest than other dairy products.
Avoid only the milk products that give you problems.
Consider trying reduced-lactose milk or milk or adding an enzyme product to milk that helps digestion. Such enzyme products are also available in pharmacies in capsule, pill or liquid drop form.
Try calcium-fortified, non-dairy drinks and foods, which you can identify by food labels. And speak with your health practitioner or registered dietitian about whether a calcium supplement could be beneficial. NOTE: These supplements can cause bloating and constipation.
Eat more calcium-rich vegetables, including broccoli and greens. If eating broccoli gives you gas, try other calcium-rich vegetables like kale, spinach, arugula and collard greens.
Cancer patients often associate a particular food with the onset of unpleasant symptoms. This phenomenon is called “acquired food aversion.”
Avoid eating your favorite foods when you know you’re likely to feel sick. That way you will enjoy your favorites during times you’re feeling well.
Remember that your food aversion will pass. In the meantime, focus on eating healthy foods you do like.
Soreness in the mouth or throat can result from cancer treatment or for other reasons. See your health practitioner to ensure that the soreness is not due to an infection. If soreness is a side effect of cancer treatment, it will generally clear up in time.
Tips
- See your dentist before beginning cancer treatment or between treatments to help prevent dental problems.
Prepare easy-to-swallow foods and include high-calorie and high-protein foods if you are having difficulty maintaining your weight. Cook foods until they are soft and tender and cut them into small pieces, or choose foods you can mash, blenderize or purée.
Serve foods cool or at room temperature, which can be less irritating than foods that are either hot or cold. For some, cold foods such as sherbet or popsicles may soothe soreness.
Drink through a straw.
Avoid alcohol, which can irritate the cells lining your mouth.
Rinse your mouth several times a day with water or a baking soda mixture. Avoid commercial mouthwashes, that often contain alcohol, instead opting for an alcohol-free mouthwash.
Consider a medication to alleviate pain before meals or a product to numb your mouth and throat while you eat. Your doctor can prescribe a medication, special mouthwashes, anesthetic lozenges or sprays.
Use a soft toothbrush. Or, if your gums are sensitive, clean your teeth with cotton swabs or mouth swabs made especially for this purpose.
Remove your dentures if your gums are sore, except while eating, and keep your dentures clean.
Don’t smoke.
Tell your doctor immediately if your gums bleed during treatment, or if you see small white patches in your mouth. These symptoms will require a visit with your dentist or a periodontist as they may signal an infection that needs attention.
Foods to try:
Bananas, applesauce, watermelon, canned fruits, peach, pear and apricot nectars, cottage cheese, yogurt, milkshakes, mashed potatoes, macaroni and cheese, custards, pudding, scrambled eggs, oatmeal
Foods to avoid:
Hot and spicy foods, alcohol, hard to chew foods
A dry mouth is most common after chemotherapy and radiation therapy to the head or neck area. A dry mouth due ti a reduction in the flow of saliva can make it difficult to chew and swallow and may change the way food tastes.
Stimulate saliva by sucking on lemon-flavored, sugar-free candies, frozen grapes, sugarless popsicles, ice chips or cubes, and try tart foods and beverages such as lemonade in small amounts.
Opt for easy-to-swallow, moist foods such as those with broth, gravy, sauces and salad dressings.
Avoid salty foods and alcohol.
When drinking, sip through a straw, and have thick beverages such as fruit nectars at room temperature or chilled.
Practice good oral hygiene. See tips under “Sore Mouth” relating to rinsing your mouth and brushing your teeth.
Keep your lips moist by applying ointment or balm.
Try using a cool mist humidifier, especially at night.
Don’t smoke.
If your dry mouth is severe, ask your doctor or dentist about products that coat and protect your mouth and about saliva substitutes and stimulants.
Tell your health practitioner about any small, white patches in your mouth, which may signal an infection requiring care.
If you are being treated for a head or neck cancer, you may develop trouble swallowing. Talk to your doctor to determine if your treatment is the reason. You might need to have a swallowing assessment to determine which foods and liquids you can safely swallow.
Eat small, frequent meals.
Purée foods, or thin out mashed foods using broth, gravy, milk or water.
Take deep breaths before trying to swallow, and exhale or cough after swallowing.
Drink plenty of fluids, aiming for eight 8-ounce glasses a day. Liquids at room temperature may be easier to swallow. Drink beverages between rather than during meals so you don’t feel full too quickly.
Ask your speech therapist or registered dietitian for help with: properly placing food in your mouth to avoid choking; adjusting your dietary fiber to avoid constipation or diarrhea while on a liquid diet; and effective swallowing techniques if part or all of your tongue or jawbone has been removed.
Report any choking or coughing while eating to your doctor, especially if accompanied by a fever.
Surgery or radiation therapy sometimes causes the esophagus to narrow, making it painful and difficult for food to pass through your chest area to the stomach. Your surgeon may be able to widen the opening or insert a feeding tube to bypass the constriction while it heals.
Try to drink liquids, which will pass through the esophagus more easily. Experiment with liquids of different viscosity or thickness. Thicker liquids may be easier to swallow. Try fruit nectars, pasteurized eggnog, smoothies or milkshakes if water and juice cause coughing or pain.
- Try pureed fruit and vegetable packets. These are often found in the packaged fruit section or the baby aisles.
Elevate your head while eating or drinking when lying down.
Some cancer treatments can cause tooth decay and other problems for your teeth and gums. Some changes to your eating habits may make the problems worse.
See your dentist before starting treatment, especially if you have a history of teeth or gum problems, to help prevent infection or other problems.
See your dentist regularly – more often than usual if you’re receiving treatment that affects the mouth (such as radiation to the head and neck). Inform your dentist about all medications you’re taking.
Use a soft-bristle toothbrush. Or, if your gums are sensitive, clean your teeth with cotton swabs or mouth swabs made especially for this purpose.
Rinse your mouth with warm water when your mouth and gums are sore. Also, rinse your mouth if you have vomited to remove stomach acid.
Limit excess sugar and sticky, sweet foods in your diet unless you are experiencing poor appetite or difficultly maintaining your weight.
Brush your teeth and tongue within 30 minutes after eating and drinking. If you cannot brush after each meal, then be sure to rinse your mouth with water.
Cancer Resource:
Living with Cancer
AICR knows how challenging a cancer diagnosis can be, and we know how overwhelming the search for reliable information can seem. Our detailed CancerResource Living with Cancer handbook offers patients and families a comprehensive resource hub for cancer care decisions. This easy-to-understand, evidence-based publication walks you through the steps you may take as you face cancer, and provides specific recommendations about eating and physical activity that can help you before, during and after treatment.

A Helping Hand
Other Programs and Resources
AICR offers you information and resources that can be used through every step of your cancer journey. Our programs, recipes and outreach can help you manage your health from treatment to recovery, and empower you to move confidently into the next chapter of your life.